Regional
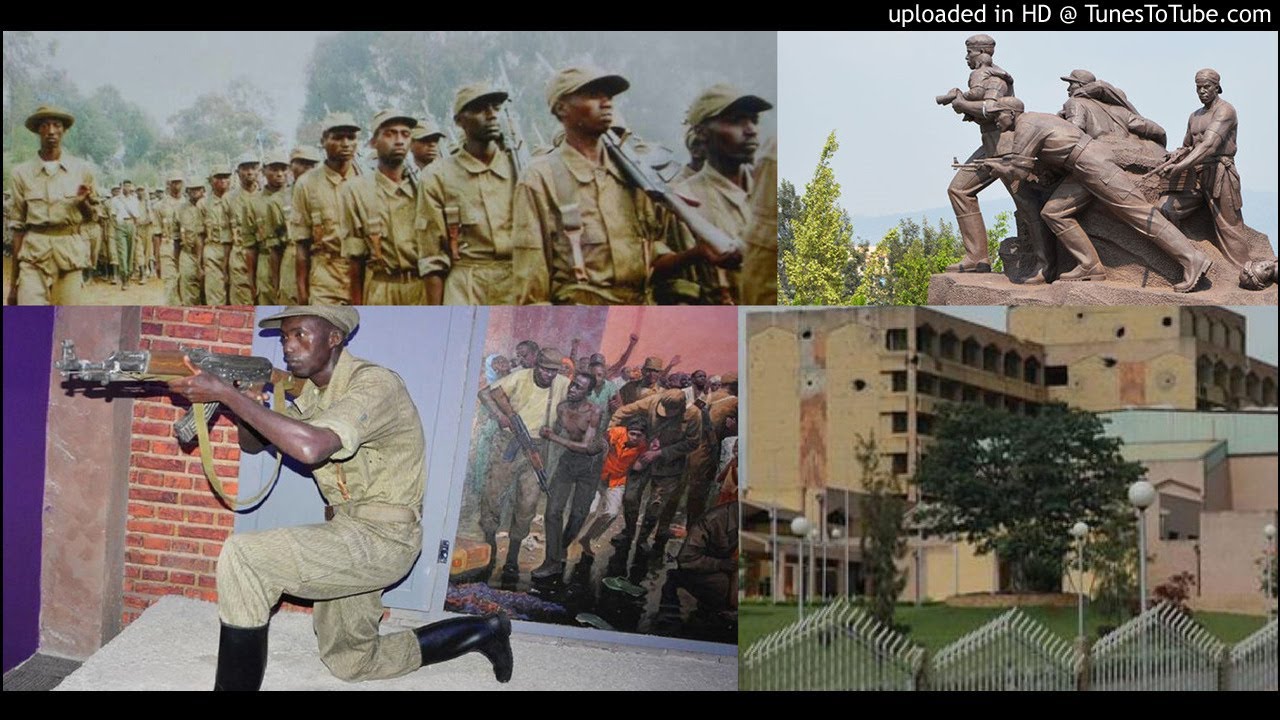
Liberation 30: Inside Rwanda’s revolutionary heath care journey

Rwanda has ensured that citizens have access to primary health care.
Thirty
years after the 1994 Genocide against the Tutsi in Rwanda, the country operates
a highly regarded universal healthcare system. Despite all the challenges,
healthcare is a right guaranteed for all, not a privilege reserved for the
rich. The country has, among others, a community-based health insurance
programme (CBHI), and more than 1,500 health posts that provide basic health
services undeserved rural communities.
Looking
back, 30 years ago, Rwanda was a devastated nation. More than one million lives
were lost in the genocide against Tutsi. Even slightly before the genocide, the
economy was ailing; with inflation at a
record 64 per cent, and a poverty rate at 78 per cent.
As of
2019, Community-Based Health Insurance, also known as Mutuelle de Sante covered
96 per cent of the population, and the
country achieved a life expectancy of 69 in 2019 from just 26 years in 1993.
According
to the WHO, Universal Health Coverage (UHC) means that “all people and
communities can use the promotive, preventive, curative, rehabilitative and
palliative health services they need, of sufficient quality to be effective,
while also ensuring that the use of these services does not expose the user to
financial hardship.”
This
success is credited to its visionary leadership, good governance, and
accountability – which led to low corruption levels, citizen participation, and
decentralization; as well as the adoption of an inclusive development model
marked by gender equality, pro-poor policies, and promotion of unity and solidarity.
Rwanda
was ranked the beacon of Universal Health Coverage in Africa by 2019. Rwanda’s
health sector agenda in general and in particular the health reforms towards
UHC have been highly valued, notably the CBHI policy and subsequent reforms
which served as the key instruments for accelerating progress towards achieving
UHC in Rwanda.
The
country has ensured that citizens have access to primary health care. The
country operates a well-functioning, decentralized healthcare public service
system comprising 1,700 health posts, 500 health centers, 42 district
hospitals, and five national referral hospitals.
Since
2000, the prevalence of child malnutrition in Rwanda has decreased from 48.5
percent to an estimated 29.8 percent. This improvement is notable, especially
considering that at one point, the figures reached as high as 49.1 percent.
When
it comes to stunting rates in Rwanda, there has been a remarkable decline over
the years, plummeting from 56.8 percent in 1992 to 33.1 percent as of 2020
according to UNICEF, WHO, and the World Bank joint global database on stunting
released on May 31.
To
further address this issue, Rwanda launched a comprehensive two-year plan on
June 12, with the goal of reducing stunting and achieving the National Strategy
for Transformation (NST1) target of reducing stunting to 19 percent by the end
of 2024.
Rwanda
targets to completely eradicate malaria by 2030, and the trend over the last
seven years gives hope that it is possible. About five million cases were
recorded in 2016, but just over 600,000 were registered last year.
The
numbers speak volumes; a reduction of severe malaria cases by 90 per cent , a
decline in malaria-related deaths by 91 per cent , and an increase in Community
Health Workers (CHWs) managing malaria cases from 18 per cent to 60 per cent.
The statistics are not just figures in a report; they represent lives saved,
families protected, and communities strengthened.
Rwanda
has undergone a remarkable journey in tackling its high maternal mortality rate
over the past decade. From an alarming 1071 maternal deaths per 100,000 live
births in 2010, the country has accelerated its rate of reduction in the MMR,
reaching 210 deaths per 100,000 live births in 2015. In recent years, the
decline has been slower, with the MMR standing at 203 per 100,000 live births
in 2020 – a decline of only 7 data points over 5 years.
The
country is currently operating at a ratio of 1 skilled health professional per
1000 population – below the WHO recommended minimum of 4 per 1000 – the
Government of Rwanda introduced a comprehensive plan designed to strengthen the
nation's health system. Known as the "4x4 Strategy", the initiative
aims to quadruple the health-care workforce over four years, while implementing
significant enhancements to health-care infrastructure and processes.
The country’s leadership is doing its best to go beyond universal primary care and develop world-class specialty healthcare services; encourage investment by specialized healthcare services providers through targeted investment promotion; and positioning Rwanda as a specialized regional medical tourism hub.







.jpg-20220704102136000000.jpg)